An abscess is a localized area of suppuration that causes pain, fever, and weakness. Often inflammation is preceded by the penetration of bacteria into the wound from the environment or secondarily through the blood. The exact cause will be determined by the doctor, hospitalization will be required - the veterinarian will monitor the pet around the clock after opening the outbreak.
Abscesses occur due to blockage of the ducts of the sebaceous glands or contamination of wounds. The disease is characterized by a gradual onset, the severity depends on the location and size of the lesion.
My cat was diagnosed with an abscess. What it is?
In simple terms, an abscess is a pocket of pus located anywhere in the body.
Abscesses are described anatomically by location, such as a tooth root abscess, submandibular abscess, soft tissue abscess of the thigh, or renal abscess. If your animal has an abscess, there will be noticeable inflammation and swelling in that area of the body, and pressing on it will be painful. The abscess may be hard or soft to the touch, like a water balloon. Of course, this applies to abscesses located on the external surfaces of the body or in the oral cavity. Abscesses that are located inside the body cavity or deep in the tissues are often not visible from the outside. The abscess may be large or small, and the skin at the site of the abscess will be red. Also, the skin at the site of the abscess may be damaged or have a fistula if the abscess begins to rupture. Breaking through, abscesses begin to emit a foul odor.
In simple terms, an abscess is a pocket of pus located anywhere in the body. Abscesses are described anatomically by location, such as a tooth root abscess, submandibular abscess, soft tissue abscess of the thigh, or renal abscess.
If your animal has an abscess, there will be noticeable inflammation and swelling in that area of the body, and pressing on it will be painful. The abscess may be hard or soft to the touch, like a water balloon. Of course, this applies to abscesses located on the external surfaces of the body or in the oral cavity. Abscesses that are located inside the body cavity or deep in the tissues are often not visible from the outside. The abscess may be large or small, and the skin at the site of the abscess will be red. Also, the skin at the site of the abscess may be damaged or have a fistula if the abscess begins to rupture. Breaking through, abscesses begin to emit a foul odor.
A cat with an abscess will often have a fever, even if the abscess has ruptured and is draining. If the abscess is located inside the body, for example, in the liver, then the animal will also have a fever, but in this case additional complications may arise in the form of purulent peritonitis, spread of infection through the bloodstream throughout the body and sepsis.
Prevention
The fight against combat abscesses is ineffective. A cat walking on the street will definitely fight, and the potential harm to health from the use of sedative drops and tablets exceeds the danger caused by suppuration. If the cat is well fed with ready-made premium food or higher, he will cope with the infection on his own.
If a cat has an unpleasant smell from his mouth, a yellowish-brown coating is found on his gums, his teeth are cleaned at the clinic and he is prescribed Hills t/d therapeutic food.
The granules contain an increased amount of fiber with organized fibers that remove plaque from the gums and teeth. Nutrition gives the cat a feeling of fullness, prevents obesity and urolithiasis.
Prevention of abscesses of the paraanal glands consists of regular cleaning, quarterly deworming, and providing adequate nutrition with ready-made premium food or higher.
What are the causes of abscesses?
There are many potential causes of abscesses in cats. One of the most common causes is a bite from another animal. A bite is a penetrating wound to the skin by teeth that are infected and the wound also becomes infected. The same principle applies to the formation of abscesses when cats scratch each other. An abscess can also occur when the skin and mucous membranes are damaged by spikelets of grass, tree branches and other sharp objects. At the same time, the wound itself is not as noticeable at the moment the animal receives it, as the abscess is noticeable after its formation. Abscesses do not always appear with bites and injuries; it depends on the depth of the wound and what bacteria got into the wound.
The following are the types of bacteria that often lead to abscesses:
- pus-forming bacteria such as Staphylococcus, Escherichia coli, some types of Streptococci, Pseudomonas aeruginosa, Mycoplasma, Pasteurella multocida, Corynebacteria, Actinomycetes, Bartonella;
- anaerobic bacteria that can only develop in the absence of oxygen, for example, Bacteroides, Clostridia, and Fusobacteria.
Pathology of the salivary glands
Nicholas Delbari
The appearance of ptyalism in an animal raises the assumption of damage to the salivary glands. Inflammation with the formation of mucocele is a fairly common occurrence that requires surgical treatment. Other pathologies of the salivary glands, which are much less common, are also described in this article.
The salivary glands are susceptible to numerous lesions, which are mainly provoked by mechanical disturbances at the level of the vestibule of the oral cavity. After an excursion into anatomy and physiology, we will look at the main diseases and treatments currently used.
Anatomy of the salivary glands
Cats and dogs have 5 pairs of salivary glands (Fig. 1).
| 1. M. digastricus 2. Gl. mandibularis. 3. V. jugularis externa. 4. M. sternohyoideus. 5. Lobus caudalis (gl. sublingualis monostomatica). 6. Lobus rostralis (gl. sublingualis monostomatica). 7. Ductus mandibularis. 8. M. geniohyoideus. 9. M. mylohyoideus. 10. Chapter sublingualis polystomatica. | 11. Radix linguae. 12. Chapter zygomatica. 13. Ductus sublingualis major (gl. sublingualis monostomatica). 14. N. lingualis. 15. N. mandibularis. 16. Ductus parotideus (beginning of the duct of the parotid gland). 17. Chapter parotis. |
The parotid salivary gland (glandula parotis) is small (the second largest among the other glands), granular and triangular in shape. This organ is covered with a connective tissue capsule and is a complex alveolar-tubular gland of the proteinaceous (serous) type. The salivary gland is located at the base of the ear between the posterior edge of the lower jaw and the wing of the atlas. The back of its base has a recess for the auricle, which copies its surface. The excretory duct (stenon duct) has a very thin wall. It emerges from the mandibular edge of the gland, obliquely crosses the surface of the large masticatory muscle (m. masseter) and opens in the form of a low nipple (papilla parotidea) into the buccal region, which is called the vestibule of the oral cavity (vestibulum oris), at the level of 3-4 or 5 molars in a dog and 2 molars in a cat. Sometimes accessory glands persist along the excretory duct.
The submandibular (mandibular) salivary gland (glandula mandibularis) is large, disc-shaped (rounded), light yellow in color. It is located shallowly in the submandibular space, partially covered by the parotid salivary gland and lies ventral to the latter. Saliva is secreted through Wharton's duct, which has thickened walls and exits near the frenulum linguae.
The sublingual salivary gland is located rostrolateral to the base of the tongue (in the sublingual fold of the mucous membrane of the floor of the mouth - plica sublingualis). It, unlike other glands, does not have a well-developed capsule and is divided into two lobules: anterior multiductal and posterior single-ductal. The posterior one (gl. sublingualis monostomatica) is emptied through the main (Bartholian) sublingual duct, which mainly exits along with Wharton's duct. The anterior multiductal sublingual salivary gland (gl. sublingualis polistomatica) is less developed, is present in all animals and is located medial to the lateral lingual muscle. Its excretion is carried out through 8-12 excretory ducts of Rivinus, which flow into the Bartholian duct or open through openings located lateral to the cranioventral edge of the frenulum of the tongue on the papilla. In cats, the posterior lobe of the sublingual gland is absent.
The buccal (molar) glands (gl. buccales) are divided into dorsal and ventral (gl. Buccalis dorsales et ventrales). It should be noted that the dog does not have a ventral buccal gland. The dorsal buccal gland is displaced towards the orbit of the eye medially from the zygomatic arch, as a result of which it received the name zygomatic gland (gl. zygomatique). It has 4-5 small excretory ducts (or one large duct of Nyuk), which open into the buccal space at the level of the last upper molar (molar).
Function and role of the salivary glands
The saliva of dogs and cats is represented by a serous (protein) part, produced by the parotid salivary gland, and a mucous part, which is produced by other salivary glands.
Physiologically normal saliva is colorless and odorless, with a pH of about 7.5. Compared to that in humans, it contains a higher amount of urea (0.1-0.3 g/l). Saliva contains sodium, potassium and some calcium, as well as albumin, mucin, amino acids, traces of glucose, vitamins, enzymes (lactoferin, lysozyme, lactoperoxidase) and immunoglobulins A. Its secretion is caused by both taste (submandibular and sublingual salivary glands) and mechanical (parotid salivary gland) irritants.
Saliva performs the following main functions:
- moisturizes the oral cavity;
- participates in thermoregulation, which is very important in carnivores;
- participates in the digestion of food;
- plays the role of a lubricant in the oral cavity to ensure the rapid passage of large quantities of food.
- secretes substances of endogenous (urea, estrogens) and exogenous origin (iodine, mercury, antibiotics, etc.);
- protects teeth.
Teeth protection is ensured as a result of:
- mechanical circulation, which is facilitated by the movement of the tongue, cheeks, and wetting with mucin;
- physicochemical properties of mucin, which includes microorganisms, immunoglobulins A (Ig A), which creates local immunity, as well as calcium salts that protect the endodont (Endodont (Gr. endon, inside; odous, odontose, tooth) [English endodentrium ] Dental pulp.);
- the presence of urea, which also plays a role in the prevention of caries.
Methods for studying the salivary glands
Ptyalism, manifested by excessive secretion of saliva or its accumulation in the cavity of the salivary glands, is the most common sign of their damage.
The examination of the animal is preceded by the collection of anamnesis (volume of saliva secreted, observation of the animal while drinking and eating food). The parotid and submandibular salivary glands are palpated through the skin, the sublingual and zygomatic glands are examined in an animal under anesthesia. Functional assessment of the salivary glands can be performed by applying a drop of atropine, intended for ophthalmic examination, to the animal's tongue. In a healthy dog or cat, we note the manifestation of profuse salivation, which is explained by the bitter taste of the drug used.
A simple x-ray examination is necessary to detect stones (sialoliths) in the salivary glands. Contrast radiography (sialography) can detect damage to the salivary glands or excretory ducts. It is performed on the animal under general anesthesia. In this case, the Telebrix contrast agent (Telebrix 35) is injected into the salivary duct using a catheter to collect urine from the cat at the rate of 1 ml/kg of body weight. The catheter is easily inserted into the duct of the submandibular and parotid glands.
Damage to the salivary glands
Lesions of the salivary glands in cats and dogs can be classified as congenital, traumatic, inflammatory and oncological.
Disorders of salivary secretion A specific study has not been conducted on the incidence of disturbed salivary secretion and salivary duct atresia in dogs. Hypersalivation with dilatation of the duct of the parotid salivary gland of a congenital nature was described in two dogs. In a young animal, excessive ptyalism is mainly accompanied by impaired lip formation.
Injuries to the glands Injuries to the parotid salivary glands or their excretory ducts are rarely diagnosed, since their scarring mainly occurs spontaneously. Sometimes the appearance of a fistula is noted. Most often this is associated with bites, surgery on the ear canal (resection, amputation), as well as otitis media, abscesses in the molar area or dental treatment.
Treatment involves repairing the damaged salivary duct or ligating it with a non-absorbable thread. In this case, the gland gradually atrophies.
The submandibular gland, encapsulated in fibrous tissue, is rarely injured.
The most common cause of damage to the salivary glands is mucocele (accompanied by accumulation of saliva).
Mucocele (lat. mucus; gr. kele, tumor) [English. mucocele]. — 1° Tumor that forms from the mucous membrane (glands of the urethra). — 2° A tumor that forms in the lacrimal sac, when there is a disturbance in the conductivity of the lacrimal canaliculi and obstruction of the nasal canal.
The accumulation of saliva occurs in the cavity of the salivary glands, which do not have sufficient elasticity of the walls to ensure evacuation (this is mainly noted in the sublingual gland). Toy breeds, as well as poodles and German shepherds, are predisposed to developing this pathology. The cause of mucocele formation has not been established (it may be due to trauma or persistence of a foreign body). Clinically, the disease is manifested by the development of edema (photo 1) or swelling of tissue under the tongue (ranula, or so-called retention cyst), which is sometimes damaged by friction against the teeth. In this case, the tongue moves to the side in relation to the damage (photo 2). In some cases, difficulties are noted during the acts of swallowing and breathing.
| Photo 1. Mucocele in a Labrador: You should pay attention to the swelling at the base of the tongue. | Photo 2. Bloating of the sublingual tissue with the development of a mucocele. |
Diagnosis of mucocele is carried out by palpation (a soft and non-painful formation) and using a puncture biopsy (the macroscopic picture when taking material from the formation is characterized by the presence of a viscous serous-hemorrhagic fluid). Placing and staining the slide with PAS confirms the presence of mucus. In some cases of chronic mucoceles may have a solid consistency without the formation of fluid. In this case, they can be confused with cysts, abscesses, stones and neoplasms. Differential diagnosis is based on radiographic examination and analysis of a sample obtained by needle biopsy.
Treatment of mucoceles is mainly performed surgically. Aspiration of the contents can sometimes provide temporary remission for several weeks or months. This manipulation is complemented by the prescription of antibiotics (clindamycin, spiramycin + metronidazole) and anti-inflammatory drugs. This therapeutic approach is intended for animals with an increased risk of anesthesia (upper airway obstruction due to mucocele, edema, anorexia, etc.) or in cases where the owner refuses to undergo surgery for the animal.
Sometimes it can be difficult to identify the affected side. Therefore, careful palpation of an animal under anesthesia should precede surgical treatment. If conditions permit, then sialography is necessary.
Salivary gland cysts can be cured using marsupialization. Part of the wall of the mucocele is excised, then a suture is placed on the oral mucosa and on the inner wall of the ranula (retention cyst). The application of interrupted interrupted sutures of absorbable thread (Vicril 3.0) is quite sufficient to ensure that the artificially formed fistula is constantly open. However, relapses occur quite often due to the closure of the surgically created fistula after a few months. Consequently, the most promising treatment for mucoceles in the pharynx, as well as ranulae and neoplasms at the base of the tongue, is complete extirpation of the salivary mandibular, sublingual glands and their ducts.
Marsupialization _ marsupialization]. A surgical method of opening the cavity of a cyst or abscess into the external environment (artificial creation of a fistula). A suture is placed on the edge of the excised surface of the skin, to which the edges of the open cavity of the cyst or abscess are sutured after partial extirpation.
Excision of the mandibular salivary glands is carried out as follows. The animal is placed in a dorsolateral position with the affected side facing the operating surgeon. A pillow is placed under the neck to better identify the glands and the relief of bone tissue (photo 3). The bifurcation of the linguofacial (v. linguofacialis) and maxillary (v. maxillaris) veins is detected by pressing on the jugular vein. A rostrocaudal skin incision of about five centimeters in length begins from the caudal edge of the lower jaw, following the direction of the bisector of the angle formed by the two veins (photo 4). The cutaneous muscle of the facial surface and neck (m. cutaneus colli et faciei), which is also called the superficial constrictor of the neck (m. sphincter colli superficialis) or platisma, is dissected and the preparation continues until we find a pearlescent fibrous sac . The linguofacial vein (v. linguofacialis) must be identified and protected. The mandibular salivary gland is grasped and pulled forward using an Alice forceps (Figure 5). Its excision continues rostrally (forward) in the direction of the salivary duct. At this stage, manipulation should be carried out with particular delicacy so as not to perforate the wall of the mucocele. Excision is complicated by the need to follow the boundaries of the gland itself. Small arteries and veins that irrigate the gland are isolated by ligation or coagulation.
| Photo 3. Excision of the mandibular gland: the location of the skin incision and the position of the animal. | Photo 4. Excision of the mandibular gland: visualization and excision of the gland. |
| Photo 5. The mandibular salivary gland is fixed and pulled back. | Photo 6. Excision of the mandibular gland: it is necessary to protect the nerves and blood vessels. |
By preparing between the digastric (m. digastricus) and chewing (m. masseter) muscles towards the tongue, the islands of the sublingual single-duct glands are brought out. This approach requires care not to damage the sublingual (n. gypoglossus) and lingual (n. lingualis) nerves, as well as the vascularity of the tongue itself (Figure 6).
Intermittent knotted sutures are placed on the capsule; The subcutaneous and skin layers are sutured in the classical way. Some authors recommend installing a Penrose drain for a period of 3-5 days. The drainage is brought out through a separate skin incision so as not to interfere with the healing of the main surgical wound. A sublingual mucocele is treated in a similar manner, but instead of a Penrose drain, the resulting pocket is marsupialized (Figure 7).
| Photo 7. Treatment of sublingual mucocele using marsupialization. |
Retroorbital (postorbital) mucocele is treated by aspiration and excision of the zygomatic salivary gland. The animal is prepared for surgery as in the previously described case. The skin is cut parallel to the dorsal edge of the zygomatic arch (arcus zygomaticus). After resection of the periosteum, it is retracted dorsally. More or less complete resection of the zygomatic arch facilitates access to the eye area. Preparation and subsequent excision of the zygomatic salivary gland, localized in the periorbital adipose tissue, is carried out after ligation of its duct. The periosteum and skin are sutured in the classical way.
In the postoperative period, the animal is prescribed antibiotics (rovamycin 50 mg/kg/day and clindamycin 11 mg/kg/day) and anti-inflammatory drugs (dexamethasone 0.1 mg/kg/day). The food is wet for a week.
Complications manifest themselves in the form of swelling under the tongue, which lasts for several days. It is necessary to monitor possible bleeding, in some cases they resort to repeated intervention to establish drainage.
Relapses are rare (1-5% of cases). This is due to the appearance of a mucocele on the opposite side or the omission of one of the single-duct sublingual glands. In any case, repeated surgical intervention is undertaken with additional sialography or by injection of methylene blue dye into the duct of the glands.
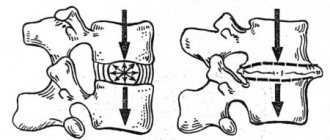
Removal of sialoliths, treatment of inflammation and abscesses Sialolith is a stone formed in the salivary duct, consisting of phosphates, calcium carbonates or magnesium (rarely found in dogs). Sialoliths can block the salivary duct and cause a painful reaction. Some foreign bodies can also cause stone formation. In such a situation, the gland often undergoes atrophy.
Stones can be identified by palpation or radiographic examination. Treatment is carried out by dissecting the salivary duct to remove the stone, or removing the entire damaged gland.
Inflammation and abscesses of the glands Inflammation of the salivary glands is extremely rare in dogs and cats. It can occur in the mandibular glands, since these glands are enclosed in a rigid (hard) capsule, which provides only slight dilatation of the organ. Any inflammation quickly leads to necrosis. According to some authors, the cause of this disease is a viral infection. The animal develops a strong pain reaction while eating food or during manipulation.
Conservative therapy (antibiotics, anti-inflammatory drugs) provides only minor improvement. Surgical treatment sometimes leads to the animal’s recovery, but in most cases, after the operation, the pain reaction persists for a long time, which necessitates a decision on euthanasia. Histomorphological analysis in all cases indicates the development of necrosis.
Abscesses of the head or neck may affect the salivary glands. In this case, inflammation and an acute pain reaction develop. Treatment is based on draining the abscess and prescribing antibiotics.
Tumors of the glands Tumors of the salivary glands are very rare (0.2% of cases). On average, their appearance corresponds to the age of ten years of the animal. These tumors are palpated at the level of the throat or oral cavity; in some cases they can cause deformation of the eyeball.
Tumors of the salivary glands mainly affect the parotid and mandibular salivary glands (Figure 8). We are mainly talking about malignant neoplasms: adenocarcinoma (50% in dogs, 85% in cats). They are primary and metastasize to nearby lymph nodes, as well as the lungs, liver, pancreas, bone tissue and adrenal glands.
| Photo 8. Tumor of the mandibular gland. |
Treatment is based on excision of the salivary glands and regional lymph nodes, as previously described. It should be noted that excision of the parotid gland is a rather complex operation, since its boundaries are difficult to determine. In addition, it is necessary to find the facial nerve (n. facialis) and isolate it. Relapses occur quite often after six months. Radiotherapy, if surgical treatment has proven to be ineffective, is possible and gives good remission for an average of 26 months. Radiation therapy in combination with surgery significantly reduces the risk of tumor recurrence in dogs and cats. The results of chemotherapy are currently unknown.
Diseases mediated by impaired immunity Some autoimmune diseases can lead to a decrease in salivary secretion (Sjögren's syndrome, which in humans is mainly combined with the manifestation of keratoconjunctivitis sicca (KS), rheumatoid arthritis and xerostomia5). Sometimes similar cases have been described in the veterinary literature. These signs are found in 20% of dogs susceptible to SBS: xerostomia manifests itself (severe periodontitis, dry mouth, decreased saliva production). Such disorders respond positively to the use of corticosteroid therapy.
Sjogren's syndrome (S. Henrik; Gougerot, 1925; Hower, 1927; Sjorgen 1933) [English. Gougerot-Houwer-Sjorgen syndrom] Syn. Orbital-articular-salivary syndrome, ophthalmic-rhinostomal-xerotic syndrome (Greyx et Levy, 1948), xerodermatosteosis (A. Touraine, 1950), sicca syndrome, dry eye syndrome, conjunctivitis sicca (Gougerot), keratoconjunctivitis sicca, and syndrome Sjögren. This syndrome most often appears in women after 40 years of age and is characterized by a decrease and then a stop in the secretion of the lacrimal, salivary, tracheal, digestive and vaginal glands. Clinically, this is manifested by generalized dryness of the mucous membranes with the development of keratitis, conjunctivitis, rhinitis, dry pharyngitis, hypertrophy and then atrophy of the salivary glands. The chronic course of the pathological process, sometimes with moderate exacerbation, is often associated with rheumatoid polyarthritis. This disease is also called Mikulicz syndrome. It is included in the classification of autoimmune diseases (sometimes associated with some of them) and diseases surrounded by immune reactions. The serum of these patients sometimes contains antitissue antibodies.
Conclusion
The pathology of the salivary glands is mainly characterized by an inflammatory process of the mucocele type. To achieve optimal results, diagnosis should be made as early as possible. Treatment of these diseases is carried out mainly by surgical intervention.
SVM 3/2004
Rate material
Like Like Congratulations Sympathy Outrageous Funny Thoughtful No words
3
Tags
Diagnostics Surgery
How are abscesses treated?
Treatment for an abscess depends on its location and the severity of the infection. Most abscesses are treated on an outpatient basis. First, the abscess is opened and drained surgically, and in addition to removing pus from the abscess cavity, necrotic tissue and sometimes the foreign object that caused the abscess are removed. If a foreign object causes an abscess, it is important to make sure that it is completely removed from the cavity, otherwise the abscess may recur.
It is important to provide adequate pain relief during abscess treatment.
Antibiotic therapy is one of the most important components of successful treatment of an abscess, regardless of its location. Antibiotics are selected based on the results of bacterial culture, i.e. those to which the bacteria are sensitive or, in the absence of such a study, broad-spectrum antibiotics are used. It is important to use the antibiotic for the entire period prescribed by the attending physician. It is also important to provide adequate pain relief during abscess treatment.
During treatment in cats, it is necessary to ensure that the animal is adequately fed. This is very important for a quick recovery. Your veterinarian may prescribe a special diet during treatment.
It is also important to confine the active animal to the space to allow the wound to heal as quickly as possible. This is especially important if the abscess was opened surgically and drainage was installed in the wound or a bandage was placed on the animal.
How to care for a cat during treatment?
During the healing of an abscess, it is important to ensure that the wound is well drained and that the drainage is not clogged, for example, with dried blood. If the abscess is internal, then it is necessary to monitor the condition of the animal and its temperature. In case of any deterioration, you should immediately contact a veterinary clinic.
Recurrence of abscesses depends greatly on where the abscess occurred and what tissues were involved. For example, in the case of anal gland abscess, the gland may need to be removed. And in the case of prostate abscess, castration of the animal can prevent relapse. It is also very important to ensure that your animal does not take part in fights (for example, in a dispute between cats for a female), this can lead to repeated abscesses.
Untimely or inadequate treatment of an animal can lead to chronic suppuration of tissues or even an organ. Therefore, it is important to follow all orders and recommendations from your veterinarian.
Opening the abscess and providing adequate drainage, followed by proper care and appropriate antibiotics, plus good pain management and nutrition, should result in a full recovery for your pet.