What is rabies
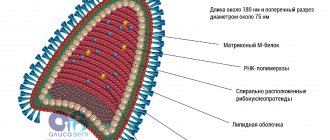
The disease is caused by the Rabies virus from the rhabdovirus family. Its main feature is its breeding site. It prefers nerve cells instead of the bloodstream, which interferes with the immune response. The action of the protective cells does not extend beyond the circulatory system, so the spinal cord and brain are completely vulnerable. If the central nervous system is seriously damaged, the infected person dies due to cardiac arrest.
The virus is able to survive at low and high temperatures for some time. The only dangers for it are ultraviolet radiation, direct rays of the sun, some disinfectants and prolonged heating. Rabies are killed by boiling for two minutes and heating to 56°C for fifteen minutes.
Incubation period
The duration of the latent period depends on the state of the immune system, as well as the location of the bite.
The virus spreads through nerve tissue at a speed of 0.3 cm/hour. The closer to the head, the sooner the symptoms will develop.
From the moment of the bite until symptoms appear, it takes from 3 days to 7 weeks.
After a single bite, the virus can circulate in the body for up to a year, and appear when the immune system weakens due to stress or illness. However, an infected dog can shed viruses in its saliva.
Methods of infection
Pets become infected from the saliva of infected animals, where the viral agent enters through parasympathetic fibers. Most often, the disease is spread by wild animals: raccoons, foxes, wolves, bats and hedgehogs. In urban areas, the danger comes from stray dogs, cats and rodents.
The most common method of infection is a bite. You can also become infected by eating an infected animal or getting its saliva on the damaged surface of the skin and mucous membranes.
Answer
It is believed that a dog is man's friend. It won’t offend the owner, much less a small child. Behaves with dignity in human society, when treated properly. A pet dog will not cause serious harm; you need to understand what happened. Why did the child suddenly get bitten? Probably, the baby’s attention was too intrusive, or the child touched a sore spot.
Now the task is not to justify the action of the animal, if the dog is domestic, it is logical to assume that the animal is vaccinated against rabies. This means that the aggression is not caused by an illness in the pet.
Stages of the disease
The infected person becomes dangerous in the early stages shortly after infection. It is very difficult to recognize the disease at the initial stage, since there are no symptoms yet. This is due to the long incubation period.
Incubation period
On average, the incubation period for rabies in dogs is 1-3 months. Its duration depends on:
- Age
. Puppies are especially vulnerable. If in adult pets the virus may not show signs of life for almost a year, then in babies everything becomes obvious already on days 5-7.
- Size and significance of the infected area
. The most dangerous place for a bite is the head. It is easier to reach the nerve endings here. A dog bitten on the head will live less than one bitten on the leg.
- Number of viral agents
. The more viruses that have entered the body, the more damage they will cause.
Regardless of what an infected dog looks like, it becomes a carrier of infection already 5-10 days after infection. This is due to the way the virus reproduces.
After entering the nerve fibers, the infection seeks to reach the cerebral cortex. While in the central nervous system, the viral agent actively creates copies of itself, affecting all internal organs. Having reached the salivary glands, it is released along with saliva and can harm others.
Even a vaccinated pet has a chance of infection. This is possible if the vaccine was administered more than six months ago. By this time, the immune response has weakened and may not be able to cope with too many pathogens.
initial stage
The first symptoms and signs of rabies in dogs are accompanied by sudden behavioral changes. Most often, sick pets become aggressive and lose fear of humans. They attack living and inanimate objects, clinging to them with a death grip. This causes their teeth and even jaws to break.
The period of aggression gives way to melancholy, when the dog tries to hide from light and noise. Any source leads to a repeated outbreak of aggression. When attacked, an infected dog does not bark, but may howl or wheeze.
The name of the disease - hydrophobia - is explained by another characteristic symptom - the fear of water. Panic horror is caused not only by the water sources themselves, but also by the noise of the pouring liquid. This is explained by a spasm of the larynx, which can kill the patient during watering.
Final stage
If a pet is sick for too long, then the reaction to external stimuli disappears. He becomes apathetic and weak. His seizures and breathing become more frequent. Soon the dog dies from laryngeal paralysis or cardiac arrest.
How many days does a rabid animal live?
After the incubation period, the infected animal shows signs of rabies. If the disease manifests itself, you should not approach the sick animal yourself and check for symptoms. It is possible to harm yourself if your pet attacks and bites. At a minimum, it will simply scare you, at a maximum, it will infect you. There is an urgent need to call a veterinarian to your home; the doctor knows how to deal with a sick dog.
There are three forms of rabies - violent, silent and atypical - the symptoms are similar, the lifespan of a sick dog varies from 2-4 to 11 days. Then the infected animal dies.
How to identify rabies in dogs: signs
The symptoms of the disease depend on the form. Not all animals are aggressive. Some become overly affectionate or simply fall into apathy soon after infection. In both cases, a change in behavior should alert the owner, since it will certainly differ from the usual.
In addition to behavior changes, watch for the following symptoms and signs:
- hanging skin and disheveled wool;
- photophobia and hydrophobia;
- rapid breathing;
- protruding ribs;
- diarrhea and vomiting;
- protruding tongue;
- chills and fever;
- cloudiness and redness of the eyes;
- refusal to eat and impaired swallowing reflex;
- muscle weakness and unsteadiness of gait.
The bite site is very itchy, so the dog constantly scratches to get rid of the irritation. If the oral cavity is damaged, itching is eliminated by actively chewing bones or furniture.
In domestic animals
Pets can become infected from street animals. The infection is also spread by rats.
If the dog has stopped responding to your voice and is constantly hiding in secluded corners for no serious reason, call the veterinarian. This behavior requires mandatory verification.
In street animals
Homeless animals are especially dangerous because no one monitors changes in their behavior. You can recognize a sick dog only by a sagging jaw, slanted eyes and hanging foamy saliva.
After meeting an infected person, try to avoid contact at all costs. Sick dogs do not warn of an attack by barking, growling or pressing their ears back. The attack will be sudden, so you shouldn’t tempt fate and test your luck.
Be sure to contact your veterinarian. Otherwise, other people or their pets will suffer.
Who can get rabies?
Rabies affects almost all species of terrestrial mammals, primarily carnivores (families canines, felines, mustelids, raccoons, etc.). Wild and domestic birds, rodents, and bats can also get sick. Every year in our country hundreds of cases of the disease are recorded among wild (foxes, raccoon dogs, wolves, etc.) and domestic (dogs, cats, cattle, horses) animals. There have been isolated cases of hydrophobia with fatal outcomes among people. The source of rabies is a wild animal that became infected in the natural environment, as well as a domestic animal that was attacked by another sick animal (wild or domestic). Humans become infected from sick animals.
Forms of rabies in dogs
Veterinarians identify 5 forms that determine how rabies manifests itself in dogs. The most common is violent, occurring in almost all infected people. Rare ones include atypical and abortive. There is a chance of sudden recovery only with the last of them.
Violent and its stages
This form lasts 5-11 days. It includes 3 stages:
- Prodromal
. The dog becomes apathetic or overly affectionate. The behavior is very different from usual. Due to the lack of oxygen, the pet often yawns, swallowing air, and saliva constantly flows from its mouth. Appetite worsens and severe anxiety appears. The patient begins to avoid loud sounds and bright lights. This stage takes 1-3 days.
- Manic
. Aggression appears. The strength of grasping movements increases. The attacker is capable of crippling not only the owner, but also himself. Clenching your jaws too hard can cause them to break. Due to paralysis of the larynx, the animal's voice changes to a more hoarse voice. The saliva that comes out foams intensely. Mood swings appear. Violence and depression alternate. The patient suffers from hydrophobia and shows interest in inedible objects. The eyes become red and inflamed, and the body suffers from painful convulsions.
- Paralytic
. The pet's voice disappears. Aggression recedes. The body becomes exhausted. The lower jaw droops. The tongue hangs out of the mouth. The larynx gradually becomes paralyzed. Along with it, paralysis binds all four legs. The dog falls into a coma. Organs gradually fail. Once the heart stops or breathing stops, death is recorded.
The first and second stages take 1-3 days. The final one lasts no more than a week.
Quiet
The name of this form is explained by the lack of aggressive behavior. The disease takes away the pet in 3-5 days.
The dog becomes lethargic, but retains its appetite. Soon he begins to eat inedible objects and cough frequently. Salivation gradually increases, and problems with the swallowing reflex appear. The jaw drops and gait becomes difficult. Gradually, paralysis covers the entire body and kills the animal.
Atypical
It is characterized by long-term development and the absence of sudden changes in mood. On average, the disease lasts 3-6 months.
With this form, all symptoms that arise resemble gastroenteritis, which complicates timely diagnosis and increases the likelihood of infection of other animals and people. A bitten pet's activity decreases. He becomes lethargic and weak. Appetite decreases. Vomiting and diarrhea interspersed with blood appear.
Returnable
Accompanied by periodic remissions lasting over a week. Despite the improvement in health, each relapse becomes more severe and ultimately kills the animal. This condition can last up to six months.
Abortive
The rarest form, accompanied by spontaneous recovery. Due to the small number of favorable outcomes, the reason for the sudden recovery has not yet been found.
Publications in the media
Rabies is an acute zoonotic viral infection that occurs with the development of severe progressive damage to the central nervous system (encephalomyelitis) with a fatal outcome. Incidence: 0.01 per 100,000 population in 2001.
Etiology • The causative agent is a neurotropic virus of the family Rhabdoviridae, genus Lyssavirus, contains RNA • Virus variants: •• Street (wild), circulating naturally among animals •• Fixed, used to obtain rabies vaccines (non-pathogenic) • Virus replication occurs in the neurons of the medulla oblongata brain, hippocampus, lumbar spinal cord; accompanied by the formation of specific eosinophilic inclusions - Babes-Negri bodies (the fixed virus does not form Babes-Negri bodies) • The virus is unstable in the external environment, quickly dies when boiled and under the influence of various disinfectants; nevertheless, it can be preserved for a long time at low temperatures.
Epidemiology. Rabies is a zoonotic infection. The main reservoirs of the virus and sources of infection are sick carnivorous wild and domestic animals: foxes (the most significant reservoir), wolves, raccoon dogs, jackals, dogs, cats. Infection of a person occurs when a bite or saliva of a rabid animal gets on damaged skin. The virus is not transmitted from person to person. The most dangerous bites are on the head, neck and hands. Susceptibility to rabies is not universal, and the incidence of the disease is determined by the area of the bite by a rabid animal: with bites to the face, rabies occurs in 90% of cases, with bites on the hand - 63%, with bites to the proximal extremities - 23%.
Pathogenesis. The virus enters the human body through damage to the skin, usually through the bites of sick animals; it should be remembered that an attack by a sick animal does not always lead to the development of rabies: the frequency of registered cases does not exceed 15%, which can be explained by the relative resistance of the human body to the virus • Replication of the virus occurs in muscle and connective tissue, where it persists for weeks or months • The virus migrates along the axons of peripheral nerves to the basal ganglia and central nervous system, where it multiplies in the gray matter and migrates back along centrifugal neurons to various tissues (including the salivary glands) • Pathomorphologically, the virus causes degenerative lesions of neurons, in cells it forms eosinophilic inclusion bodies with jagged edges, predominantly in the Ammon's horn cells of the hippocampus, known as Babes-Negri bodies.
Clinical picture and diagnosis
• History: bite or contact with saliva of a rabid animal on damaged skin; information about the fate of the animal (died, is under veterinary supervision, disappeared) increases the diagnostic significance.
• Periods of disease development •• Incubation period (from 10 days to 1 year); significant variability of this period is determined by the following factors: localization of the bite (the shortest - for bites to the head, hands), age of the bitten (in children the period is shorter than in adults), size and depth of the wound •• Initial (prodromal) period: duration - 1-3 days •• Period of height (excitement): duration - 2-3 days •• Paralytic period: duration - 1-3 days • Total duration of the disease - 4-7 days, in rare cases - 2 weeks or more.
• Clinical symptoms •• In the prodromal period of the disease, the first signs are found at the site of the bite: the scar swells again, turns red, itching and pain appear along the nerves closest to the site of the bite. General malaise, low-grade body temperature, sleep disturbances are noted •• The period of the height of the disease ••• Attacks of hydrophobia, occurring with painful convulsive contractions of the muscles of the pharynx and larynx, noisy breathing, sometimes stopping breathing when trying to drink, and later at the sight or sound of pouring water , verbal mention of her. Attacks can be provoked by air movement (aerophobia), bright light (photophobia), loud sound (acoustophobia) ••• The appearance of the patient during an attack: he throws his head and torso back with a scream, throws his trembling hands forward, pushes away a vessel with water; inspiratory dyspnea develops (the patient inhales air whistling). The attacks last a few seconds, after which the muscle spasms go away ••• Attacks of psychomotor agitation: patients become aggressive, scream and rush around, break furniture, showing superhuman strength; the development of auditory and visual hallucinations is possible; increased sweating and profuse salivation are noted; the patient cannot swallow saliva and constantly spits it out ••• Autonomic disorders: mydriasis, tachycardia, arterial hypertension ••• Increased body temperature •• Paralytic period ••• Calmness: fear, anxiety and melancholy, attacks of hydrophobia disappear, hope arises for recovery (ominous calm) ••• Paralysis of the limbs and damage to cranial nerves of various locations ••• Increased body temperature above 40 ° C ••• Autonomic disorders: sweating, arterial hypotension, bradycardia, etc.
• Death occurs from cardiac arrest or paralysis of the respiratory center.
Research methods. Laboratory confirmation of the diagnosis is possible only posthumously based on the following methods: • Detection of Babes-Negri bodies in horn cells • Detection of rabies virus Ag in cells using immunofluorescence analysis and ELISA • Conducting a biological test with infection of newborn mice or Syrian hamsters with the virus from the saliva of patients, suspension of brain tissue or submandibular glands • It is fundamentally possible during the patient’s lifetime to isolate the virus from saliva or cerebrospinal fluid, as well as to test the reaction of fluorescent antibodies on corneal prints or skin biopsies, but in clinical practice this is difficult to achieve, and the diagnosis is based on the clinical manifestations of the disease.
Differential diagnosis • Tetanus • Atropine poisoning • Dissociative disorders • Viral encephalitis.
Treatment. There is no specific therapy. Symptomatic and supportive treatment is carried out (hypnotics, anticonvulsants, painkillers, parenteral nutrition, etc.).
Prevention • Combating the source of infection (compliance with the rules for keeping cats and dogs, preventing straying among them, preventive vaccination of domestic animals against rabies, control of the population of wild animals) • If bitten by a suspicious animal, it is necessary to immediately provide assistance to the victim. The wound and areas wetted with the animal’s saliva should be thoroughly washed with a stream of water and soap, the edges of the wound should be treated with iodine tincture, a sterile bandage should be applied, the edges of the wound should not be excised or sutured during the first three days (except for life-threatening ones); it is necessary to ensure immunization against rabies • For active immunoprophylaxis, dry inactivated cultural rabies vaccine RABIVAK-Vnukovo-32, dry inactivated concentrated purified cultural rabies vaccine and rabies immunoglobulin are used •• Detailed schemes of therapeutic and prophylactic immunization for each vaccine take into account the severity of the bite and the nature of contact with animals (salination, settling, etc.), information about the animal, etc. Vaccination is effective only when the course begins no later than the 14th day from the moment of the bite •• Vaccinations are carried out unconditionally (for bites of clearly rabid animals, in the absence of information about the bitten animal ) and conditional (if bitten by an animal without signs of rabies and if it is possible to observe it for 10 days) indications •• If a short incubation period is suspected (extensive lesions of soft tissues, localization of the bite close to the brain), active-passive protection of the victim is carried out : in addition to the vaccine, rabies immunoglobulin is also administered. The duration of intense post-vaccination immunity is 1 year.
ICD-10 • A82 Rabies • Z20.3 Contact with a sick person or the possibility of contracting rabies • Z24.2 Need for immunization against rabies
Risk of infection from a dog
Humans are also warm-blooded animals, so the risk of infection is very high. The most dangerous places for a bite are the hands, neck and face.
Soon after infection, the bitten person experiences a headache, slight fever, diarrhea, vomiting, cough and general malaise. As the disease progresses, neurological disorders and paralysis are added. Without timely help, a person dies.
If rabies is suspected
Avoid contact with potentially dangerous animals and call a doctor. If your pet is infected, isolate it in a separate room until doctors arrive.
What to do if you are bitten by a rabid dog
The wound should be washed as soon as possible with running water and a thick soap solution. This should be done not only if you are bitten, but also if you receive a scratch or saliva gets on the skin. After treatment, lubricate the affected area with an antiseptic and apply a bandage.
If the bleeding is weak, do not block it, but allow some of the blood to drain before washing. This will remove some of the saliva and reduce the concentration of the virus.
In addition to your veterinarian, contact an emergency room immediately. For a favorable outcome, characteristic signs of infection must not be allowed to appear. The victim will have to receive 6 injections in the shoulder area over 3 months. The virus is suppressed by immunoglobulins or rabies serum. In the first case, the drug pre-contains antibodies that attack the infection, and in the second, the body produces them on its own.
What preventive measures are there if you are bitten by an animal?
All kinds of recommendations for the prevention and treatment of rabies - the destruction of enraged animals, cauterization of bitten areas in people with a hot iron - did not produce any effect. Almost every person bitten by a rabid animal was doomed to death. Until the 80s of the 19th century, people did not have a reliable means of protection against this terrible disease.
The great French scientist Louis Pasteur has the honor of creating a vaccine against rabies, which was successfully used for the first time on July 6, 1885. Then, thanks to vaccination, a boy bitten by a rabid dog was saved. And some time later, in a French village, children playing were attacked by a rabid dog. Defending them, fifteen-year-old shepherd Jean Jupille accomplished a real feat. He managed to tie the dog's face with a belt whip and kill it with his wooden shoe. But the boy's entire body was covered with wounds. Barely alive, Jean was brought to Paris. Pasteur saved the hero.
To this day, vaccinations remain the only reliable means of protecting people after being bitten by an animal sick or suspected of having rabies. These include the administration of a vaccine and, if necessary, immunoglobulin.
What you need to know about preventive vaccinations:
- if the doctor has prescribed vaccinations, they should be started immediately;
- Under no circumstances should you skip the next vaccination;
- the course of vaccinations prescribed by the doctor must be completed in full;
- a person who is vaccinated is not dangerous to anyone;
- During vaccinations, you should not drink alcoholic beverages for 6 months after their completion; you should avoid overwork, hypothermia, and overheating.
Along with vaccinations, on the recommendation of Belarusian scientists, antibiotic prophylaxis is also carried out.
Diagnostics: rabies test
To exclude other similar diseases, blood is taken from the dog for ELISA or PCR analysis. There is also a rapid test that determines the presence of the virus in saliva. These diagnostic tests are performed very rarely. They are not only dangerous for doctors due to the threat of infection, but also uninformative due to frequent false negative results.
The only reliable diagnostic method is to examine brain tissue. It is carried out posthumously to confirm which disease the four-legged patient died from. If the result is positive, the analysis shows the presence of Babes-Negri bodies - neoplasms that appear in the brain when infected with the virus.
Other changes are noticeable only at autopsy. An accumulation of exudate is found in the spinal canal, and numerous hemorrhages are found in the stomach and cerebral convolutions.
Immediately after contacting the veterinarian, the animal is placed in a closed box for up to 1 month. The four-legged patient continues to be fed, monitoring changes in condition. If there is a sudden improvement and no relapses, the dog is considered healthy.
Is it possible to cure rabies in a dog?
Once symptoms of rabies are diagnosed in dogs, treatment and any other contact are excluded. Despite the low probability of an abortive form, the patient is euthanized immediately after the onset of hydrophobia and paralysis. A cure for the disease has still not been found, so this is the only humane solution to ease further suffering.
Before symptoms appear, the dog is vaccinated twice. The second time the vaccine is administered 2 weeks after the first injection. In the absence of characteristic signs, preservation of the same state of health and a negative result of a rapid test for the presence of the virus, the animal is considered healthy.
Frequently asked questions about rabies vaccinations
A reliable way to protect yourself from rabies is to get vaccinated.
In areas unaffected by rabies, the veterinary service is required to conduct door-to-door visits and vaccinate all dogs and cats. However, it is not easy to complete such a task. Therefore, take care of the dog’s health yourself.
Dogs living in high-rise apartments are least likely to be in danger. Rabies infection threatens primarily hunting dogs, as well as dogs living in the vicinity of forested areas.
If you are going to travel with your pet, participate in expert exhibitions, or engage in breeding, you are required to obtain a veterinary passport. The document must contain a note about vaccination against rabies.
How long does the vaccine last? How often should I do it?
Adult dogs are immunized annually.
Instructions for the use of rabies vaccines produced in Russia recommend vaccinating puppies from eight weeks of age. Abroad, they adhere to the rule of vaccinating cubs no earlier than 84 days.
To form strong immunity in young animals, one or two vaccinations will be required.
In response to vaccination, antibodies are produced, the viruscidal concentration of which remains for 3 years.
Your dog will not be allowed to breed or show if its last vaccination was more than a year ago.
When does a puppy get its first vaccination?
If you have purchased a puppy, vaccinate it. Clinically healthy pets are allowed to receive vaccinations. Instructions for use of most vaccines recommend that the first immunization be given to an eight-week-old baby. Revaccinate after 3-4 weeks.
Try to use vaccines from the same manufacturer. I recommend vaccinating puppies with polyvalent drugs. If possible, get immunized before replacing baby teeth with permanent teeth. If changing teeth is accompanied by discomfort, reschedule the revaccination.
How to prepare a dog
The dog must be absolutely healthy. 2 weeks before the proposed vaccination, free your pet from fleas, and 7 days from worms. Parasites interfere with the formation of immunity and contribute to the occurrence of post-vaccination complications.
Protect the unvaccinated animal from contact with its yard relatives.
Feed your pet nutritious food, preferably premium ready-made food or higher. Do not change food, do not introduce new ingredients, limit treats.
3 weeks before vaccination, do not use antibiotics or hyperimmune serums. Do not feed your pet before vaccination.
The veterinarian examines the dog and conducts thermometry. If it is elevated or the dog is found to be unwell, the procedure is postponed to another time.
To prevent an allergic reaction, an antihistamine is administered. Do not rush to leave the clinic. Observe your pet’s behavior for a quarter of an hour so that you can provide him with emergency assistance if complications arise.
Watch the video:
Where to get vaccinated?
Read the instructions carefully. Most biological products are administered subcutaneously, in the withers area, or intramuscularly in the thigh.
If you are using an inactivated monovaccine against rabies, treat the injection site with 70% alcohol.
When vaccinating with a complex preparation, it is impossible to moisten the skin with alcohol before the injection - the living weakened components of the biological product will die.
On topic: How to give an injection to a dog
Can a vaccinated dog get rabies?
Vaccination reliably protects your pet from rabies, however, it does not provide a 100% guarantee.
A breakdown of immunity occurs in the following cases:
- The rules of transportation and storage were violated. If you purchase the vaccine, make sure it is stored in the refrigerator. Transport in a thermos with ice. The biological product cannot be frozen.
- The expiration date has expired.
- The drug was not administered to the place indicated in the instructions.
- The injection was given to a non-dewormed or sick dog.
- An animal that is in the incubation period of infection was vaccinated.
- The dog has a congenital defect that prevents the formation of immune bodies.
During the USSR, medicines for dogs were obtained. In the nineties, biological products began to be produced at the research institute. I learned about the production of a medicine that has an antiviral effect. I called and found out how to purchase. I was informed that an employee of the company was going to pass by my city on vacation in Sochi and would bring biological products. It was summer, the travel time was 3 days. I boarded the train, after the conversation I bought some immunoglobulin and distributed it to my friends. One veterinarian complained that the medicine did not work. Apparently, due to the fact that the transportation regime was violated.
What side effects and complications are possible?
The dog is injected with an antigen, even if it is killed. Therefore, the body reacts to the appearance of a stranger, due to which antibodies are formed against this virus.
Normal post-vaccination complications include the following symptoms:
- hyperthermia, 0.5° above normal;
- lump at the injection site;
- malaise;
- one-time refusal to eat;
- single vomiting or short-term diarrhea in the absence of bloody discharge;
These symptoms are typical for puppies that are being vaccinated for the first time. Adult pets tolerate the vaccine without clinical manifestations.
Vaccination.
Quarantine after vaccination
The concentration of antibodies increases gradually and reaches a viruscidal value 3 weeks after vaccination in puppies and 2 weeks after vaccination in adults. During this time, limit your pet's stay outside.
During this period, provide peace to the dog, do not create stressful situations, and do not change the diet.
Do not wet the injection site, do not bathe your pet, and limit physical activity.
How much does it cost on average?
The state program for combating especially dangerous infections of animals and humans requires free vaccination against rabies for the entire population of dogs and cats in areas affected by rabies.
However, owners of purebred dogs prefer to vaccinate their pets with commercial vaccines, because cheap Russian-made biological products do not enjoy a high international reputation. Veterinarians at government agencies are not interested in immunizing outbred livestock.
In private clinics, the average cost of vaccination is 500 rubles.
They produce monovalent bivalent and complex vaccines.
The cost of vaccinations against rabies ranges from 100 to 200 rubles.
The price of polyvalent biological products ranges from 250 to 700 rubles.
At the clinic, there is a markup on biological products. Therefore, expect the cost of an anti-rabies vaccination to be 800 rubles, a complex Russian-made vaccine to be 1000 rubles; imported - 1500 rub.
In the dog's passport, they make notes about vaccination.
How to protect your dog from infection
The main method of prevention is timely vaccination. All other methods are considered additional. They also reduce the likelihood of infection, but are effective only when used in combination.
Vaccine
The first vaccination is given to the puppy at 3 months or after the appearance of the molars. All subsequent vaccinations are carried out annually.
A persistent immune response appears only after the 3rd injection, but even then it does not provide one hundred percent protection. Vaccinated pets receive the right to participate in exhibitions and can freely travel outside the country.
The main reason for refusing this preventive measure is the price. Not all owners have the opportunity to pay for the vaccine annually. As an alternative solution, veterinarians advise contacting government clinics, where the procedure is carried out free of charge using domestic drugs.
Before vaccination, the four-legged patient is treated for parasites and checked for diseases. It is not recommended to vaccinate a sick, pregnant or lactating animal. This can lead to infection due to too weak an immune response from the exhausted body.
Can a vaccinated animal get sick?
The immune response lasts up to a year, but weakens within six months after vaccination. It is from this moment that the vaccinated pet becomes more vulnerable to infection. Rare cases of infection account for only 2-4%.
After an attack on a vaccinated dog, prepare a veterinary passport with notes on the vaccines administered. He is also vaccinated and isolated for a certain time until the circumstances are clarified. If vaccination was carried out recently, and your pet managed to scratch or bite you, the administration of anti-rabies serum is not practiced.
With timely treatment, the likelihood of death is almost zero. The existing immunity and an additional dose of serum are guaranteed to get rid of the infection.
What to do if your dog is bitten by a suspected rabies carrier
Immediately after a bite or other injury, first aid is allowed. For your safety, be sure to wear protective gloves and use a muzzle. After this, proceed with the following steps:
- Remove hair from the damaged area with scissors.
- Wash the wound with plenty of soapy water. Use a syringe to remove some of the saliva by squirting the liquid under pressure.
- Isolate your pet in a separate room and call a veterinarian. The pet will be taken into temporary quarantine to ensure its safety for others.
Don't ignore the attack that has occurred. If you are not sure about the health of the attacked animal, then do not try to check the possible consequences in practice. Temporary isolation will not harm your pet, but will only help avoid a fatal disease.
How can a person be saved from being infected by the rabies virus?
Absolutely every person should know what to do if bitten by a dog with rabies. And it doesn’t matter so much whether it’s your own or a homeless one. So, the actions should be like this:
- If the bite occurred in an area protected by clothing, you need to quickly determine whether the fabric is torn or not. If the dog's teeth reach the body, you need to firmly squeeze the skin around the bite, squeezing out a little blood along with infected saliva;
- The wound should be washed and treated with iodine, brilliant green or hydrogen peroxide;
- You should immediately contact a medical facility to donate blood and take a smear from the cornea to confirm or refute the diagnosis;
- The hospital will need to give consent for the administration of rabies vaccine and immunoglobulin. Moreover, all the specialist’s instructions must be followed strictly, otherwise the virus can cause irreparable harm to the body.
Rabies is not a disease that can be taken lightly. Once visible signs of illness appear, it will no longer be possible to save a person’s life. Treatment will be aimed only at reducing the patient's suffering. Ideally, after any bite from a stranger or your own dog, it is better to immediately contact a specialist.